Abstract
Background: While dCBT is associated with high rates of sustained donor engraftment, delayed neutrophil recovery in adults is frequent and can contribute to extended hospitalization and early transplant-related mortality.
Methods: We investigated engraftment after myeloablative dCBT supplemented with CD34+ selected haploidentical PBSC (haploCD34+) in patients (pts) with high risk hematologic malignancies or aplastic anemia in a phase II clinical trial. The aim was to abrogate neutropenia (ANC >/= 500 within 14 days) with a haplo myeloid bridge prior to CB engraftment. Pts did not receive ATG due to the increased mortality risk reported in adult CBT. Double unit CB grafts allowed comparison to dCBT controls without haploidentical graft supplementation.
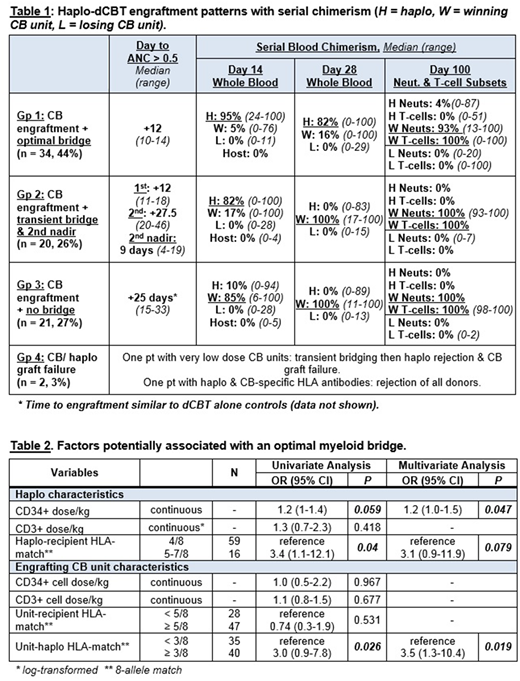
Results: 78 adult pts [median age 48.5 years (range 21-68), median weight 82 kgs (range 48-138), 44 (56%) CMV+, 3 with prior allografts] underwent haplo-dCBT between 9/2012-12/2017. Diagnoses included 54 (69%) acute leukemias, 10 (13%) MDS/ MPN (all ≤ 10% blasts at work-up), 10 (17%) NHL/ HD and 1 aplastic anemia. Conditioning was myeloablative (1 Cy 120/ Flu 75/ TBI 1375, 77 intermediate intensity Cy 50/ Flu 150/ Thio 5-10/ TBI 400) with CSA/ MMF. CB units had a median infused TNC of 2.3 (range 1-5.7) x 107/kg/unit & median infused viable CD34+ cell dose of 1.1 (range 0.1-3.1) x 105/kg/unit with a median 5/8 (range 2-7) unit-recipient HLA-allele match. Haplo CD34+ grafts [procured from children (46%), siblings (31%), parents (13%) or extended family (10%)] had a median infused CD34+ dose of 5.2 x 106/kg (range 1.1-16.8) and a median infused CD3+ dose of 1.6 x 103/kg (range 0.3-13.7). Sixty-one (78%) haplos were 4/8 and 17 (22%) were 5-7/8 HLA-matched to the pt. In 77 evaluable pts (1 pt died on day 14), 4 engraftment patterns were observed (Table 1). All but 2 pts had sustained CB engraftment with either an optimal haplo-bridge (Gp. 1, 34/77, 44%), a transient bridge with a second nadir preceding CB engraftment (Gp. 2, 20/77, 26%), or no bridge (Gp. 3, 21/77, 27%). The 2 remaining pts had CB/ haplo graft failure (Gp. 4, 2/77, 3%); both were successfully re-transplanted with single CB units. While there was no difference in the day 100 TRM in the 34 optimal bridge pts vs pts with transient or no bridge [9% (95%CI 2-21) vs 15% (95%CI 6-27), p = 0.388], optimal bridge pts had faster platelet recovery [19 (range 14-41) vs 44.5 days (range 14-67)] and earlier hospital discharge [28.5 (range 20-60) vs 36 days (range 28-98)]. Similar to dCBT alone, chimerism analysis revealed sustained engraftment in haplo-dCBT is mediated by a "winning" CB unit. This was heralded by winning unit-derived T-cells seen as early as day +28. Although universal, the speed of haplo rejection varied, and a high haplo chimerism percentage early post-transplant did not guarantee successful bridging. Analysis of factors potentially predicting an optimal bridge is shown in Table 2. The median winning CB unit-haplo 8-allele HLA-match was 3/8 (range 1-7/8). In univariate analysis, higher haplo CD34+ dose/kg, > 4/8 haplo-recipient HLA-match and ≥ 3/8 winning unit-haplo HLA-match were associated with a higher likelihood of bridging. Haplo CD34+ dose and winning unit-haplo HLA-match remained significant in multivariate analysis.
Conclusions: While haplo-dCBT can be associated with enhanced neutrophil recovery, this platform does not guarantee a successful myeloid bridge due to early haplo rejection by the winning CB unit. This universal haplo rejection highlights the importance of the CB graft dose and quality with this ATG-free strategy as the CB will mediate sustained engraftment. Our findings have significance for strategies that combine unmanipulated CB with any third-party or ex vivo expanded T-cell depleted product given higher product CD34+ cell dose and better HLA-match to the unmanipulated CB unit could improve the likelihood of successful myeloid bridging. The data also support alternative approaches to improve myeloid recovery after CBT such as optimized unit selection and vivo expansion.
O'Reilly:Atara Biotherapeutics: Consultancy, Patents & Royalties, Research Funding. Perales:Takeda: Other: Personal fees; Novartis: Other: Personal fees; Incyte: Membership on an entity's Board of Directors or advisory committees, Other: Personal fees and Clinical trial support; Merck: Other: Personal fees; Abbvie: Other: Personal fees. Sauter:Juno Therapeutics: Consultancy, Research Funding; Sanofi-Genzyme: Consultancy, Research Funding; Spectrum Pharmaceuticals: Consultancy; Novartis: Consultancy; Precision Biosciences: Consultancy; Kite: Consultancy. Shah:Janssen: Research Funding; Amgen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.